There is one common thread that dominates every conversation that we have with healthcare payers and providers — the desire to provide improved care at lower costs. Are you feeling the constant pressure to improve spend and efficiencies within your network?
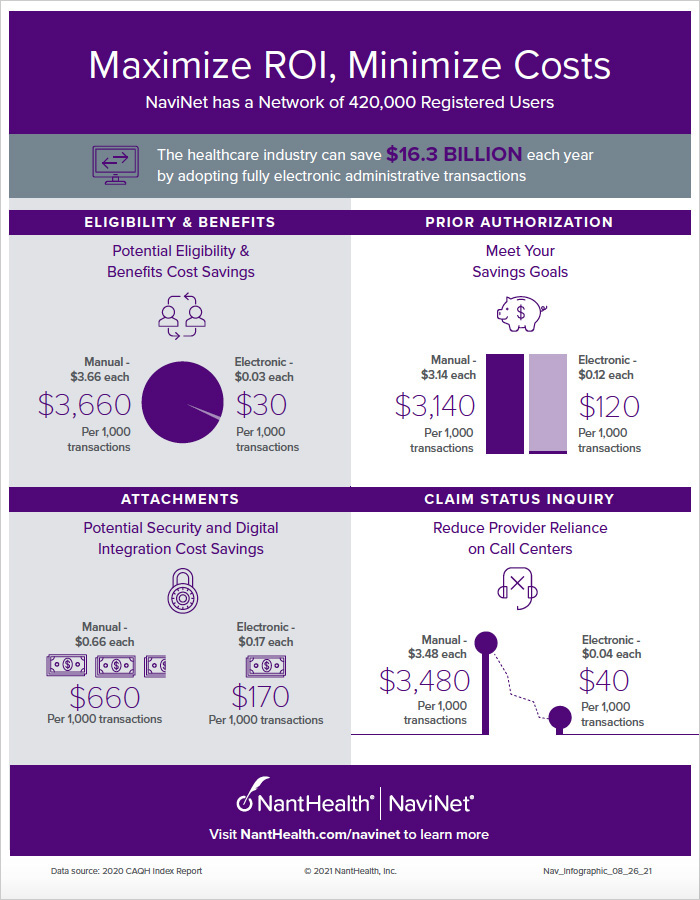
Many providers are still relying on costly and time-intensive manual approaches to handle their documentation requirements or to coordinate care. The providers in your network are not alone. This is a major industry issue tracked by the CAQH Index, which found that out of the $39 billion spent each year conducting administrative transactions, 42% of that amount or $16.3 billion could be saved by transitioning to fully electronic transactions.
The most common questions we get from our health plan customers typically land in one of these four categories — if not all four. Do these sound familiar?
- How can our organization partner with others to better provide access to eligibility and benefits checks more efficiently?
- How can we reduce the time and costs associated with prior authorization requests?
- How can we manage attachments more efficiently and reduce the dependence on fax and manual processes?
- How can we reduce the provider time on our call centers for routine and common inquiries?
To help answer some of these questions and to give you a sense of the cost savings associated with these frequently asked questions, the NaviNet team has pulled together this benchmark guide so that you can compare the manual vs. automated time and tackle these important questions too.
Infographic: Maximize ROI, Minimize Costs
To learn more, visit www.nanthealth.com/navinet