Provider-Friendly. Payer-Focused.
Experience enhanced collaboration, reduced administrative costs, and optimized workflows.
Multi-Payer Provider Access
Providers can access workflows provided by NantHealth’s Health plan partners, or subscribe to access our nationwide network.
Rich Transactional, Interactive Workflows
Payers can configure custom workflows that align with their business requirements and goals.
Healthcare data flows both ways, in real-time
Experience modern payer-provider interoperability with timely bidirectional data flow.
NaviNet enhances payer-provider network engagement with intuitive workflows and quick access to insurance information.
Strategic Differentiators
Full-service partnership with consultative support.
Branding and messaging tools to communicate directly with providers.
Platform management and compliance handled by NantHealth.
Trusted advisory services for implementation and optimization.
Magnify your brand and keep providers informed
Your NaviNet Plan Central page is unique to you and your brand. Providers visit this centralized access point to view all workflows and resources available from your health plan in NaviNet.
You control what appears on Plan Central. Update and customize content at any time, post announcements and alerts, and share network information and resources.
I have been using NaviNet for the last 10 years. I can honestly say that it has made my work life much easier and more efficient.”
David F., Clott, Matthew – Constructive & Reconstructive Surgery
Exchange critical documents with providers
Support bi-directional exchanges of information to engage providers during vital clinical workflows with NaviNet Document Exchange.
Exchange administrative, financial, and clinical information in real-time—including care gaps, fee schedules, risk adjustment information, quality measurement data, and performance reports.
Thrive in a world of value-based care by providing access to critical information at the point of care. Learn more.
I have been using NaviNet for over 20 years and found it to be the most user friendly and informative website. This is the first website that I use to train new staff and always my ‘go to’ for all types of information.”
Debbie S., Office Manager, Hess Physical Therapy
Simplify the insurance verification process
Deliver membership verification and insurance coverage information to provider offices in real-time. Tailored to your organization’s business needs, NaviNet Eligibility and Benefits displays copayment, deductible, and benefit information, and is designed to easily extend to display more detailed information.
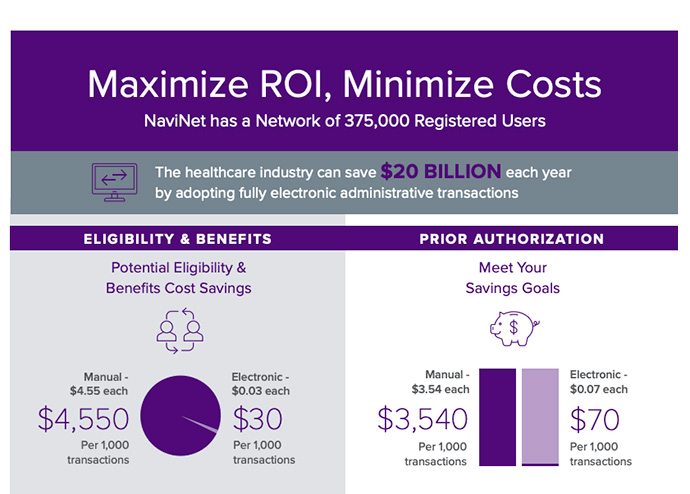
$12.8 Billion
Estimated annual savings opportunity for automating the eligibility & benefits workflow.1
37/member
Average number of eligibility & benefit verifications annually.1
Automate responses to claim status requests, reducing costs
Give provider offices access to detailed financial and claim status information in real-time, eliminating the need to call your organization directly. NaviNet Claim Status Inquiry aligns health plan and provider interests by automating the delivery of claim receipt confirmation, adjudication status, and important payment details.
$15.68 vs $2.07
Estimated cost of a manual claim status inquiry per transaction versus per electronic transaction.1
169 Million
Number of phone calls yearly between providers and health plans to verify claim status.1
Manage the entire lifecycle of a claim, digitally
Providers can submit claims directly to payers with the NaviNet Claims Management suite. NaviNet leverages clearinghouse partnerships to streamline claim submission. Claims are efficiently routed to health plans through existing clearinghouse connections, eliminating phone calls, costly paper claims, and other manual processes associated with claims follow-up, correction, and resubmission.
Save money and boost provider satisfaction through automation of claim submission, adjustments, attachments, investigations, and appeals.
169 Million
Number of phone calls yearly between providers and health plans to verify claim status.1
$2.3+ Million
Estimated annual savings potential to fully automate claims management.1
$25/per transaction
Additional cost for claims requiring rework.2
Exchange instant HIPAA-compliant authorization requests and inquiries
Increase provider trust, satisfaction, and overall network relations by shifting authorizations from a costly and time-consuming manual process to a streamlined online form submission with electronic follow-up.
NaviNet Authorizations lets providers access the most up-to-date authorization information—such as status updates, approvals or denials, and requests for additional information—online.
Configure fields, add additional business logic, and integrate with third-party applications. Add-on workflow capabilities better support necessary requirements.
Only 28%
Number of authorizations that are fully electronic.1
$3,600+
health plans savings per 1,000 transactions by shifting to electronic prior authorizations.1
Facilitate informed referral decisions
Enable provider offices to make more informed referral decisions and ensure value-based contract success by providing detailed referral information. NaviNet Referrals lets provider offices submit and access referrals in real-time, guides patients to the best specialist at the most affordable cost, and equips staff with more information to navigate complex sub-networks while you optimize in-network or value-based referrals.
1 in 3
Number of patients referred to a specialist every year.3
$10M
Amount, on average, every primary care physician controls of downstream healthcare spend.4
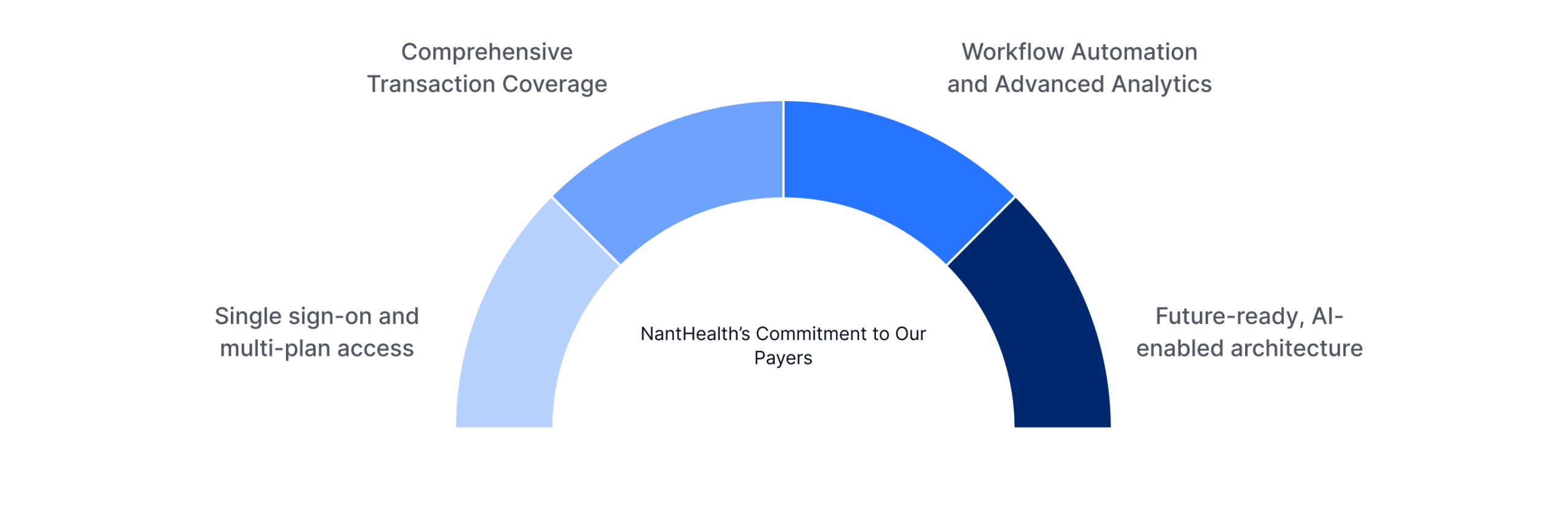
Your Vision Our Platform – Together We Deliver.
NantHealth is committed to being more than just a technology vendor – we are a trusted partner invested in your plans success.
With NantHealth, your organisation gains a partner that is:
Best in-Class & Proven
25 years of trusted delivery, nationwide scale, and zero system outages.
Simple & Reliable
We don’t overcomplicate; we aim to reduce friction and deliver tools that work seamlessly for providers.
Future Focused
Agile, innovative, and aligned with market trends to evolve with your vision.
Our customers know how important it can be to leverage technologies and data that improve patient outcomes and help them focus on member health. We believe that it’s equally important to leverage community and collective knowledge to drive innovation. As a NantHealth customer you’ll receive a dedicated team of consultants, trusted advisors, support, and training.
Provider adoption and engagement
NaviNet’s goal is to enable payers to eliminate provider friction, improve transparency, and accelerate digital transformation – consistently validated by market-leading Net Promoter Scores.
40%
Higher Adoption
48
Net Promoter Score
NaviNet aims to provide users with increased operational efficiency, streamlined communication, and significant savings. We design tools with the goal of reducing manual processes across your organization through decreased administrative complexity and increased transparency, with the desired results of timely, higher quality, more cost-effective care that directly benefits patients.
Safe, Secure, Streamlined
For NantHealth, security is a priority. NaviNet is HIPAA compliant and HITRUST certified, having met key regulations
and industry-defined requirements. It appropriately manages risk regarding third-party privacy, security and compliance.
1 2022 CAQH Index Report
2 Medical Group Management Association (MGMA)
3 Mehrotra A, Forrest CB, Lin CY. Dropping the Baton: Specialty Referrals in the United States. The Milbank Quarterly
4 Mostashari F, Sanghavi D, McClellan M. Health Reform and Physician-Led Accountable Care: The Paradox of Primary Care Physician Leadership. JAMA
5 Based on the quarterly analysis of total electronic authorization submissions through the NaviNet platform, compared to the 2024 CAQH Index Report
6 Based on ongoing simple user/customer surveys, our net promoter score (NPS) measures overall customer experience. The score is calculated by the Net Promoter Formula, Total % of promoters – Total % of detractors.