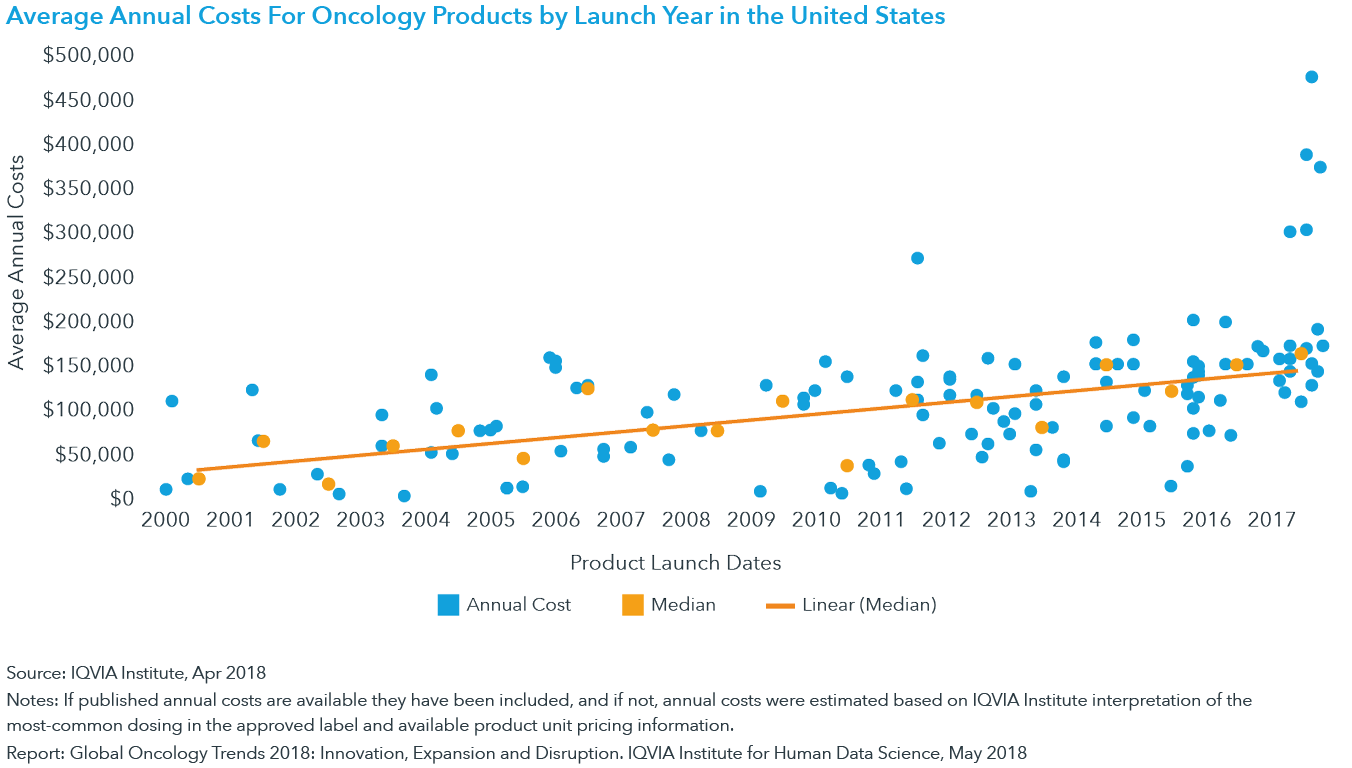
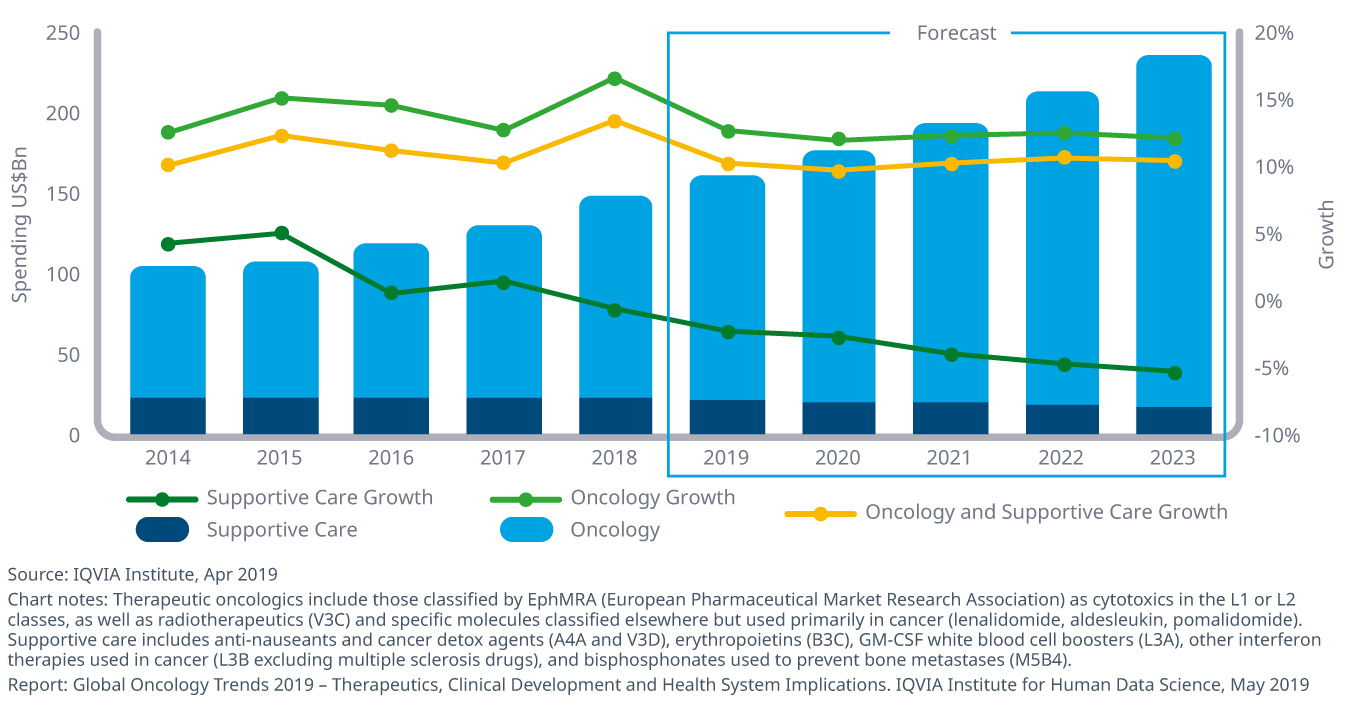
In 2018, spending on cancer drugs in the United States has more than doubled since 2013 and has now exceeded $56 billion. Today, the median annual cost of a new cancer drug launched is $149,000 and 42% of cancer patients will lose their life savings due to treatment.
In part one of this four-part series from our webinar “The Evolution of Value-Based Care: A Shift to Patient-Centric Care,” we chat with NantHealth Chief Medical Officer Dr. Bobby Reddy as he examines the rise in cancer costs and how payers can better manage these costs. Within the series, Dr. Reddy will discuss the emergence of patient-centric care, tech disrupters and the shift to digital healthcare, and how tech can help the transition to value-based care.
NH: The cost of cancer care is rising. What do you see as major concerns associated with this rise?
Dr. Reddy: The major factors that are driving costs in not just cancer care but all of healthcare are the same factors that we’ve had for the last 20, 30 years. We have very significant expenditure around treatments. As we develop new treatments, they’re inherently more expensive. Old treatments are less expensive. Generic drugs are less expensive. We are in a very exciting time in oncology, where we are going with a fundamental shift. Where we had diseases in the past that we would describe as incurable, and now we don’t describe them that way anymore. We use Jimmy Carter often as an example. Jimmy Carter is a man with an incurable disease ten years ago – metastatic melanoma to the brain is incurable. Yet, he is cured. We are in a very different time and space. In that context we can justify very high expenditure around these drugs. We are not talking about buying people four to six months; we are talking about changing their outcome and actually making them disease-free. As we have younger and younger patients faced with cancer, we can render them disease-free without long-term bad side effects that we’ve seen with chemotherapy or radiation, so that these people can return back to being productive members of society. It’s very exciting, but obviously, that cost is very significant. Unfortunately, a lot of this cost is not born directly by insurance companies. We know that bankruptcy is rampant among patients with cancer, it’s a very significant expenditure – so this is a problem that we have to solve. It’s exciting that we can come up with new therapies, potentially curative therapies, but we also have to do that in a way that’s fiscally responsible for society so that we have access to these therapies for all people.
NH: While cancer and cancer death rates have steadily dropped, drug spend is skyrocketing. When you’re talking about cancer spend and that providers are juggling a number of factors when deciding on a treatment plan for their patients, why are there so many considerations?
Dr. Reddy: There are so many factors that go into making a treatment plan for a patient. There is the clinical data piece that is difficult for any doctor – it doesn’t have to be oncology; it can be any field of medicine. That’s why people go to medical school and have to do additional years and years of training to be able to intake that information and synthesize it in a useful way and come up with an individualized treatment plan for a given patient because no two people are the same. So what are all those factors? Certainly, in the last five years, we’ve had more drugs approved in cancer than we had approved in the prior 30 years. This is a lot of information – it’s information overload for physicians as we learn about new drugs, new mechanisms of action, new underlying biological principles, new biomarkers, and new ways to group the patients. When I was in training, we had colon cancer, lung cancer, and we had breast cancer. And now, with lung cancer, you can’t describe it as lung cancer; you have to start bucketing it as driven by eGFR, driven by Alk, driven by BRAF, PD-L1 positive, PD-L1 negative. It becomes a very difficult process I think for a clinician to know everything about everything as we have more and more information about cancer.
NH: There are close to 10,000 decision data points for oncologists that may need to be considered when you look at everything, including oncologists aligning to evidence-based, best outcomes, cost, etc.
Dr. Reddy: That’s exactly right; there are so many pieces of data that you need in order to make the best possible decision. You do want to make the right decision for your individual patient, but you also want to be able to practice good, sound, evidence-based medicine and do it in a fiscally responsible manner. We have things like the NCCN as one example of guidelines, but having guidelines helps, as does tools. There are multiple tools available in the marketplace; NantHealth provides one of them as a pathway tool called Eviti. There are a variety of pathway tools out there that essentially allow a physician to interact with this huge piece of information out there – the biomarkers, the treatment plan recommendations from guidelines – and synthesize that based on the individual patient’s needs. So you can say, “I know that my patient has colon cancer and has KRAS mutated colon cancer, so what should I give them?” That’s pretty easy in the first line. But what do you do in the 2nd and 3rd lines? Now we’ve got nice pathways that can tell us that these treatments are well-established. I think most practicing oncologists are going to see those every day, but when you have a rare tumor, a very unusual sarcoma, this is going to level the playing field a bit so that the average community practicing doctor can still be able to practice good, sound, evidence-based medicine and feel confident about what they’re doing because they’ve got the tool behind them that allows them to be an expert in something that perhaps they don’t see every day.
NH: Payers can protect both their members and their bottom line by really looking at the evidence-based guidelines and aligning themselves with a tool to help sort through the “gray areas” and make sure what they’re approving for their patients is evidence-based and best practice for their members?
Dr. Reddy: That’s exactly right. Payers want the best possible outcome for their members. Obviously, a good outcome is generally going to cost less money, so that’s a good thing. It’s also a good thing, clinically, so everybody wants that. How can we better get there together? Having common, accepted pathways that both the payers get behind. If you are able to more quickly adjudicate a treatment decision, and it’s going to comport with your medical policy, why wouldn’t you want that? That allows you to say we have confidence that this individual is getting the best possible treatment that has already been essentially reviewed by our own internal medical policy team, and we know that in these clinical circumstances, these are the things that we would do. It’s bridging between having both the providers and payers, who both are stakeholders, and if we’re really going to do value-based care everybody has to be a stakeholder. They can meet in the middle and agree that these are the set treatments that we think have good evidence and economic support so that we can get behind it.
NH: What kind of implications will patient-centric value-based care have on the industry?
Dr. Reddy: Patient-centric care, this is what healthcare is anyway. It’s not really like other businesses. If you’re selling shoes, you could sell the shoe or not sell the shoe. You can’t choose not to provide healthcare. We have to provide this – this is a responsibility that we have to society. Patient-centric means that the patient is the center of a larger spoke-and-hub system that is all designed to support that individual; support them in health, and definitely in sickness when they’re going to need support. Patient-centric care means that we take into account the wishes of that individual. To do that, we need to be able to provide that individual with data – with information – so that they can make informed decisions. Everyone has their thoughts about how they want to live their life, and I think that’s important so that we respect those wishes, and people can make decisions about their healthcare as well.
*Be sure to view part 2 of our series where we take a deeper dive into patient-centric care.