Expedite the Drug Prior Authorization Process
NaviNet® Open has teamed up with CoverMyMeds® to deliver NaviNet Drug Authorizations, a free solution that helps providers electronically submit prior authorizations for any drug under any plan—including Medicaid and Medicare.
NaviNet Drug Authorizations streamline the prior authorization process by:
- Eliminating administrative waste
- Increasing provider satisfaction
- Speeding up patient access to prescribed medications—directly improving patient care
From Hours to Minutes
Drug Authorizations minimize the amount of time your staff spends on the phone and managing paper forms. Replace the prior authorization process with an efficient, online authorization request process that takes just minutes per submission.

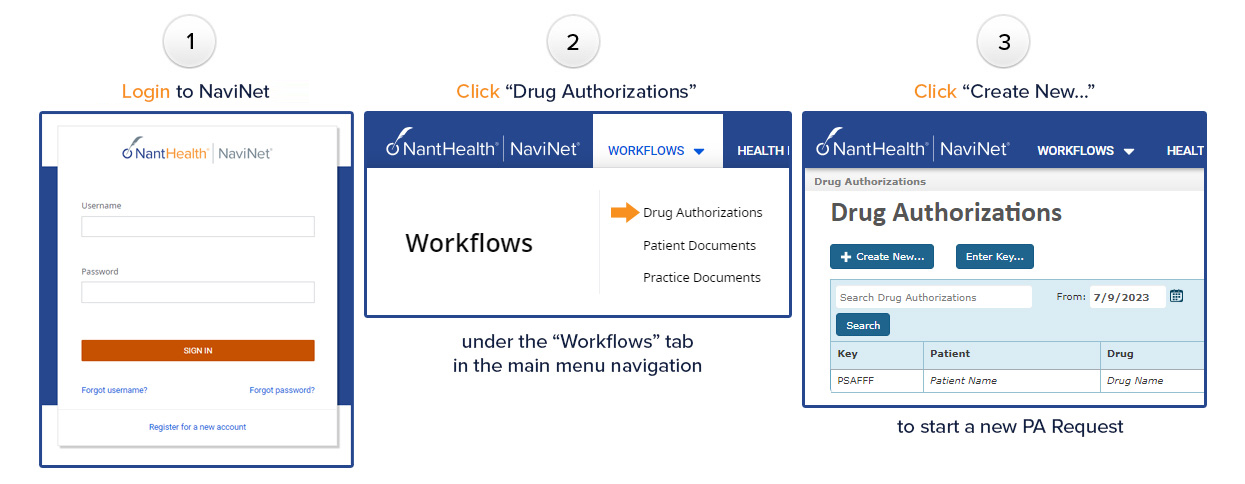
How to Start
Click Drug Authorizations under the Workflows tab in the upper left corner of the page.
Click Create New… to start a new PA request.
Benefits
- Save time with a streamlined prior authorization process
- Lower administrative costs by minimizing faxes and phone calls
- Receive faster determinations in real-time—and at no cost for prescribers and their staff
- Help keep patients on the drug prescribed by their doctor
- Reduce patient prescription abandonment
Features
- Manage all prior authorizations forms and follow up on one dashboard—regardless of the plan, patient, or drug
- Available for all prior authorizations across all plans (Medicare, Medicaid, and commercial), for all drugs
- Store patient, pharmacy, and physician demographics in address books that input directly to the appropriate prior authorization form
- Locate the proper prior authorization form—for any drug—in seconds
- Access prior authorization requests already started by nearby pharmacies and seamlessly complete them online
- Store physician’s digital signatures in the system—allowing any signature applied to a prior authorization to be faxed directly to the payer, without having to print it first












